Concussions - Athletic Trainers, Directors, and Coaches
Basic Concussion Protocols for Athletic Trainers and Coaches
What happens if a player appears concussed?
An athlete with a suspected concussion must be taken out of play immediately (per Florida legislation) and cannot return until they have obtained a written medical clearance from a neurologist or a physician trained in the management of concussions.
During the time between sustaining the concussion and seeing the doctor, it is advised that the athlete rest as much as possible, both physically and mentally.
Once the player is asymptomatic (which means symptoms have disappeared), the player's physician will advise them to begin a "Gradual Return to Play" process.
How do I tell if a player has sustained a concussion?
Read our concussion signs and symptoms in our FAQ to familiarize yourself with the signs and symptoms of a concussion.
How does Gradual Return to Play (GRTP) work?
When a physician has cleared an athlete, the athlete cannot immediately return to full-contact. Instead, a Gradual Return to Play (GRTP) checklist is implemented.
GRTP allows the player - in incremental daily steps - to re-acclimate their brain to exercise and expenditure in a safe and controlled manner.
It is important that the athlete show no signs or symptoms such as dizziness, headache, or nausea during the GRTP process; if so, the athlete must report this to their athletic trainer and return to their concussion physician for further evaluation. However, if the athlete successfully passes the GRTP checklist with no symptoms, they can return to full contact.
What is the injury reporting system, and how does it affect me?
Our concussion program tracks all sports-related, high school concussion injuries with Miami-Dade County Public Schools and the Palm Beach County School District for research and evaluation. If a player is injured in the course of their athletic activities, their respective athletic trainer, director, or principal is required to report this concussion to our program through our online injury surveillance form.
Reporting takes approximately 5 minutes. Please have dates of injury, ImPACT tests, and GRTP on hand.
Submit ReportClassroom Education
Our 15-minute video - produced in partnership with Sports Legacy Institute (now Concussion Legacy Foundation) - explains the health dangers of concussions and what teammates can do to stay safe during play or practice:
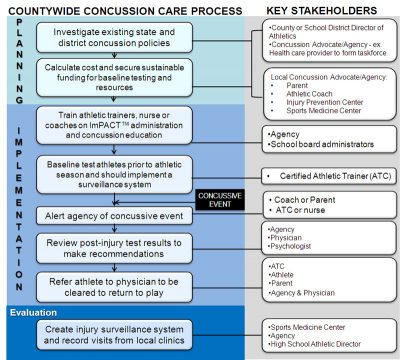
Six Steps to Play Safe - Our concussion management model
The Six Steps are a standardized order of activities for coaches, trainers, and medical professionals to use with players 13 years and older. This model is used by Miami-Dade County Public Schools and the Palm Beach County School District.
This protocol ensures all student athletes get baseline tested prior to play and that all future injuries are managed to maximize the player's safety and improve recovery.
1Pre-season baseline

Prior to play, a coach or ATC administers an ImPACT test to the athlete. The Immediate Post-Concussion Assessment and Cognitive Test is a 45-minute computer-based test that measures verbal and visual memory and reaction times. The athlete's initial test becomes their baseline in the event of a suspected concussion.
These tests are administered before the season for athletes that play contact sports. ImPACT tests are for players 13 years of age or older.
2Sideline Testing

When an athlete shows signs or symptoms of a concussion, they must be immediately removed from play.
A certified athletic trainer (ATC) must evaluate them with a sideline assessment test, such as SCAT5.
This sideline test will assist in determining if the player has actually received a concussion and whether they should be removed from play for the remainder of the game.
3Post-ImPACT Test

Within 24 to 72 hours following the injury, we recommend that ATCs re-test the concussed player with the Post-ImPACT test and inform parents to make an appointment at the UHealth Concussion Clinic to see a specialist.
4Clinic Followup

As soon as possible, parents of a concussed athlete should make an appointment for their child or teen athlete to visit our concussion clinic for the following tests, evaluations, and recommendations:
- Neurological evaluation & concussion education
- Vestibular evaluation
- Neuropsychological assessment
- Review of ImPACT scores by a Credentialed ImPACT Consultant (CIC)
- Recommendations for return to play (GRTP, RTP) and return to learn (school accommodations)
5Return To Play
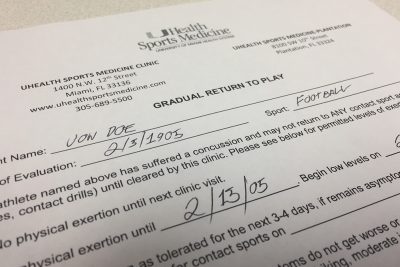
Once the athlete is completely free of symptoms and has been evaluated and examined by a physician to be asymptomatic, said physician will clear the player to begin the Gradual Return to Play (GRTP) protocol.
If the player remains symptom free following GRTP, they may return to full contact play once medically cleared (in writing) by a physician.
6Injury surveillance
Once the athlete has returned to full-contact activities, the athletic trainer will submit a concussion injury report through our site.
Submit Report